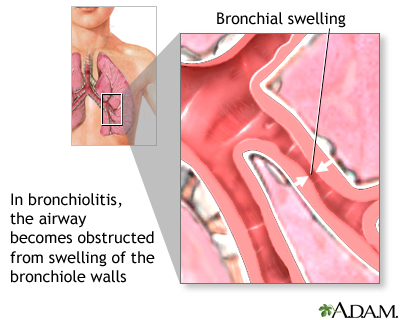
Bronchiolitis is a common illness of the respiratory tract caused by an infection that affects the tiny airways, called the bronchioles, that lead to the lungs. As these airways become inflamed, they swell and fill with mucus, making breathing difficult.
Bronchiolitis:
- most often affects infants and young children because their small airways can become blocked more easily than those of older kids or adults
- typically occurs during the first 2 years of life, with peak occurrence at about 3 to 6 months of age
- is more common in males, children who have not been breastfed, and those who live in crowded conditions
Day-care attendance and exposure to cigarette smoke also can increase the likelihood that an infant will develop bronchiolitis.
Although it's often a mild illness, some infants are at risk for a more severe disease that requires hospitalization. Conditions that increase the risk of severe bronchiolitis include prematurity, prior chronic heart or lung disease, and a weakened immune system due to illness or medications.
Kids who have had bronchiolitis may be more likely to develop asthma later in life, but it's unclear whether the illness causes or triggers asthma, or whether children who eventually develop asthma were simply more prone to developing bronchiolitis as infants. Studies are being done to clarify the relationship between bronchiolitis and the later development of asthma.
Bronchiolitis is usually caused by a viral infection, most commonly respiratory syncytial virus (RSV). RSV infections are responsible for more than half of all cases of bronchiolitis and are most widespread in the winter and early spring. Other viruses associated with bronchiolitis include rhinovirus, influenza (flu), and human metapneumovirus.
Signs and Symptoms
The first symptoms of bronchiolitis are usually the same as those of a common cold:
- stuffiness
- runny nose
- mild cough
- mild fever
These symptoms last a day or two and are followed by worsening of the cough and the appearance of wheezes (high-pitched whistling noises when exhaling).
Sometimes more severe respiratory difficulties gradually develop, marked by:
- rapid, shallow breathing
- a rapid heartbeat
- drawing in of the neck and chest with each breath, known as retractions
- flaring of the nostrils
- irritability, with difficulty sleeping and signs of fatigue or lethargy
The child may also have a poor appetite and may vomit after coughing. Less commonly, babies, especially those born prematurely, may have episodes where they briefly stop breathing (this is called apnea) before developing other symptoms.
In severe cases, symptoms may worsen quickly. A child with severe bronchiolitis may tire from the work of breathing and have poor air movement in and out of the lungs due to the clogging of the small airways. The skin can turn blue (called cyanosis), which is especially noticeable in the lips and fingernails. The child also can become dehydrated from working harder to breathe, vomiting, and taking in less during feedings.
Contagiousness
The infections that cause bronchiolitis are contagious. The germs can spread in tiny drops of fluid from an infected person's nose and mouth, which may become airborne via sneezes, coughs, or laughs, and also can end up on things the person has touched, such as used tissues or toys.
Infants in child-care centers have a higher risk of contracting an infection that may lead to bronchiolitis because they're in close contact with lots of other young children.
Prevention
The best way to prevent the spread of viruses that can cause bronchiolitis is frequent hand washing. It may help to keep infants away from others who have colds or coughs. Babies who are exposed to cigarette smoke are more likely to develop more severe bronchiolitis compared with those from smoke-free homes. Therefore, it's important to avoid exposing children to cigarette smoke.
Although a vaccine for bronchiolitis has not yet been developed, a medication can be given to lessen the severity of the disease. It contains antibodies to RSV and is injected monthly during peak RSV season. The medication is recommended only for infants at high risk of severe disease, such as those born very prematurely or those with chronic lung disease.
Incubation
The incubation period (the time between infection and the onset of symptoms) ranges from several days to a week, depending on the infection causing the bronchiolitis.
Duration
Cases of bronchiolitis typically last about 12 days, but kids with severe cases can cough for weeks. The illness generally peaks on about the second to third day after the child starts coughing and having difficulty breathing and then gradually resolves.
Professional Treatment
Fortunately, most cases of bronchiolitis are mild and require no specific professional treatment. Antibiotics aren't useful because bronchiolitis is caused by a viral infection, and antibiotics are only effective against bacterial infections. Medication may sometimes be given to help open a child's airways.
Infants who have trouble breathing, are dehydrated, or appear fatigued should always be evaluated by a doctor. Those who are moderately or severely ill may need to be hospitalized, watched closely, and given fluids and humidified oxygen. Rarely, in very severe cases, some babies are placed on respirators to help them breathe until they start to get better.
Home Treatment
The best treatment for most kids is time to recover and plenty of fluids. Making sure a child drinks enough fluids can be a tricky task, however, because infants with bronchiolitis may not feel like drinking. They should be offered fluids in small amounts at more frequent intervals than usual.
Indoor air, especially during winter, can dry out airways and make the mucus stickier. Some parents use a cool-mist vaporizer or humidifier in the child's room to help loosen mucus in the airway and relieve cough and congestion. If you use one, clean it daily with household bleach to prevent mold from building up. Avoid hot-water and steam humidifiers, which can be hazardous and can cause scalding.
To clear nasal congestion, try a bulb syringe and saline (saltwater) nose drops. This can be especially helpful just before feeding and sleeping. Sometimes, keeping the child in a slight upright position may help improve labored breathing. Give acetaminophen to reduce fever and make the child more comfortable.
When to Call the Doctor
Call your doctor if your child:
- is breathing quickly, especially if this is accompanied by retractions or wheezing
- might be dehydrated due to poor appetite or vomiting
- is sleepier than usual
- has a high fever
- has a worsening cough
- appears fatigued or lethargic
Seek immediate help if you feel your child is having difficulty breathing and the cough, retractions, or wheezing are getting worse, or if his or her lips or fingernails appear blue.