Mesothelioma is difficult to diagnose because the early signs and symptoms of the disease
can be subtle or mistaken. Symptoms are all too frequently ignored or
dismissed by people who are inclined to attribute them to common every
day ailments. Sometimes patients live with symptoms for up to 6 months
before being diagnosed but usually the symptoms are present for two to
three months prior to a mesothelioma diagnosis.
Mesothelioma is difficult to diagnose because the early signs and symptoms of the disease
can be subtle or mistaken. Symptoms are all too frequently ignored or
dismissed by people who are inclined to attribute them to common every
day ailments. Sometimes patients live with symptoms for up to 6 months
before being diagnosed but usually the symptoms are present for two to
three months prior to a mesothelioma diagnosis.
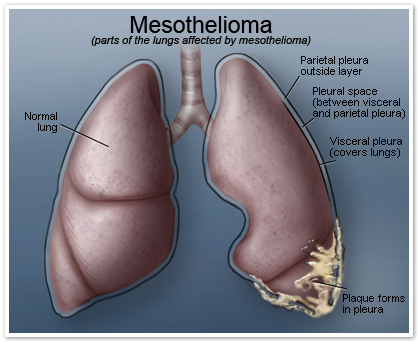
About 60% of patients diagnosed with pleural mesothelioma experience
lower back pain or side chest pain, and there are frequent reports of
shortness of breath. Lower numbers of people may experience difficulty
swallowing, or have a persistent cough, fever, weight loss or fatigue.
Additional symptoms that some patients experience are muscle weakness,
loss of sensory capability, coughing up blood, facial and arm swelling,
and hoarseness.
Peritoneal mesothelioma originates in the abdomen and as a result,
symptoms often include abdominal pain, weight loss, nausea, and
vomiting. Fluid buildup may occur in the abdomen as well as a result of
the cancer.
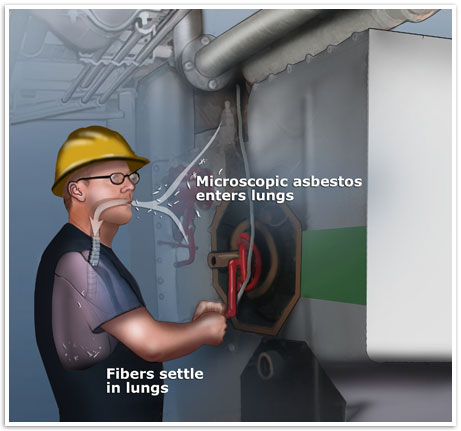
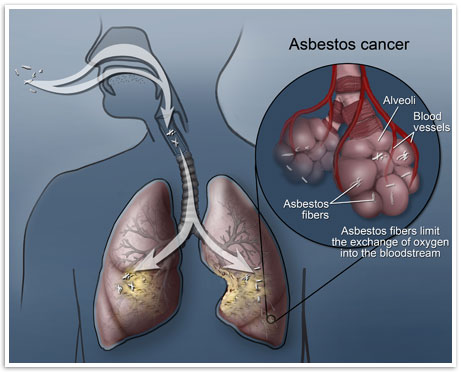
Asbestos exposure is considered the primary risk factor for the development of the cancer.
Anyone previously exposed to asbestos displaying any of these symptoms
should seek medical attention from their doctor first, only to be
referred to a doctor who specializes in the treatment of mesothelioma and thoracic oncology after receiving a positive diagnosis.
How long does it take for mesothelioma symptoms to appear?
One of the most unique facts about mesothelioma is that the disease
is characterized by a long latency period that is very often associated
with the disease. The latency period is the amount of time that
elapses from the first point of asbestos exposure to the point where
symptoms begin to appear so that a diagnosis can be made. In some
mesothelioma cases the latency period
is reported to be 10 years but the average latency for the majority of
cases is between 35 and 40 years. As a result, the cancer often
progresses to later stages
before a diagnosis is made. When diagnosed in the later stages,
mesothelioma treatment options become more limited and are less
effective.
Symptoms of Mesothelioma
Provided below is a list of symptoms that mesothelioma patients may
experience. Please click on a symptom to learn more about it.
Anemia
Mesothelioma patients diagnosed with anemia have a lower than normal red blood cell count or hemoglobin in the blood.
Blood Clotting Disorder
A symptom experienced by many mesothelioma patients that can lead to
anemia and other serious complications if not given appropriate
medical attention.
Bowel Obstruction
Bowel obstructions can be a direct effect of the cancer. It is a
very painful symptom that can sometimes develop in peritoneal
mesothelioma patients.
Chest Pain
Often experienced in pleural mesothelioma and pericardial
mesothelioma patients, chest pain can develop as the tumor grows and
places strain on the lungs and heart.
Dysphagia
Pleural mesothelioma patients often develop difficulty swallowing
(esophageal dysphagia) as the mesothelium continues to grow on the
lungs.
Fluid Effusion
An effusion can occur in mesothelioma patients when there is fluid
buildup affecting either the pleura or pericardium. This may need to be
drained in a relatively limited surgical procedure to control the
effusion and associated symptoms.
Hemoptysis
Hemoptysis, or the symptom of coughing up blood, can have its
origins in the lungs, bronchi or trachea of mesothelioma patients.
Nausea
Nausea is experienced in a number of cancer patients, as it is often
a side effect of chemotherapy treatment and sometimes the underlying
cancer. Those diagnosed with peritoneal mesothelioma may also
experience nausea as a result of increasing abdominal pressure.
Peritoneal Effusion
Peritoneal mesothelioma patients may experience a buildup of fluid
in the peritoneum as the tumor continues to grow. This can result in an
effusion which can inhibit the function of abdominal organs.
Peritoneal Effusion
In pleural mesothelioma patients, pleural effusion may develop when
there is a large amount of fluid present in the pleura, the lining
between the lungs and chest cavity.
Weight Loss
Weight loss can occur in mesothelioma patients as a side effect from
cancer treatment or as the result of other symptoms that may also be
present, such as difficulty swallowing or nausea.